Improving patient access to medicines - Affordability solutions as part of the puzzle
Improving patient access to medicines - Affordability solutions as part of the puzzle
Article written by Kristina Funk, Amy Morgan and Mattia Belloni, Windrose Consulting Group
Introduction to affordability solutions
Affordability challenges can hinder patient access to medicines in many countries, especially those with low income or limited public health coverage. Thus, pharmaceutical companies are increasingly interested in exploring patient-targeted affordability solutions to widen access in the out-of-pocket (OOP) sector. Affordability solutions are programs of varying design aimed at lightening the financial burden on patients when purchasing drugs OOP, which separates them from donation programs (where treatment is provided free of charge) and payer-targeted contracts (e.g., financial-based agreements to ease the burden on the payer).
Affordability solutions can be an interim bridge until reimbursement is achieved, or a long-term program to support patients in the absence of reimbursement. If only part of the patient population receives reimbursement, a hybrid approach might be suitable - at first the program would support patients broadly, but after some patients receive reimbursement, the solution is targeted specifically at patients remaining in the OOP sector.
In addition to increasing access in the OOP sector, these solutions allow the manufacturer to establish a presence in a market (with the opportunity to start generating revenues while optimizing the supply infrastructure as needed), increase patient and physician experience with the product, and produce real-world evidence (RWE), which can be leveraged during payer discussions to maximize reimbursement.
Defining an affordability gap
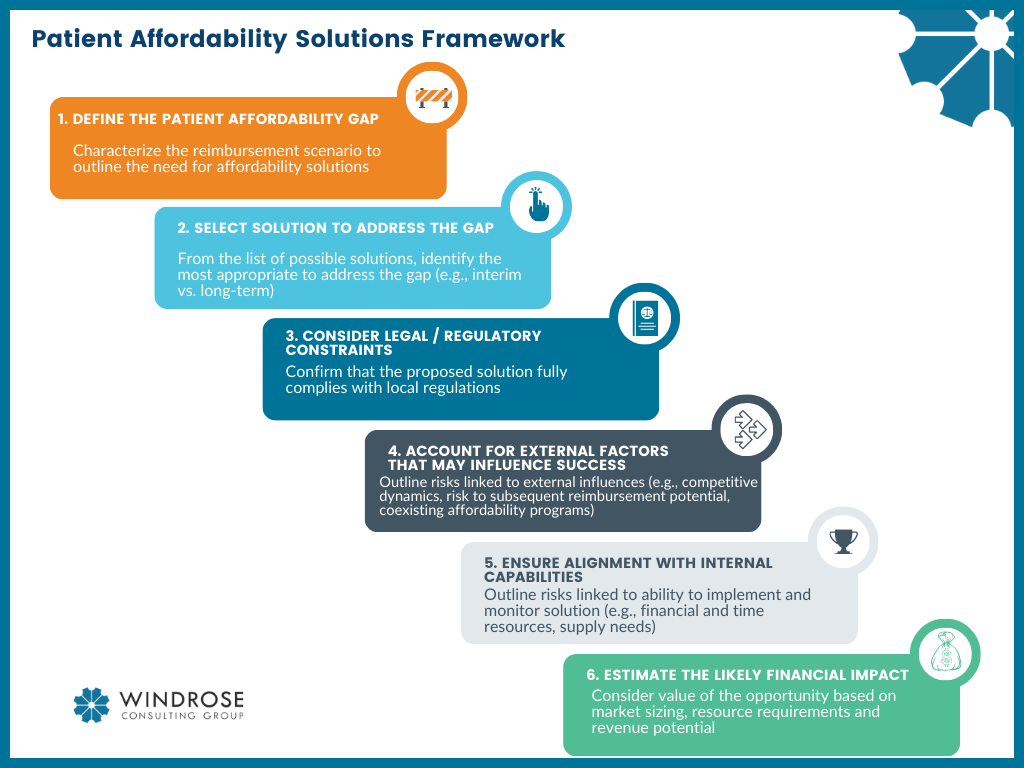
Patient Affordability Solutions Framework
To assess the need for an affordability solution, the presence of an affordability gap has to be confirmed based on three elements: the expected reimbursement outcomes (i.e., whether reimbursement will be granted to the full or part of the population), the time to reimbursement, and the suitability of “alternative access” routes, such as through the courts or charitable access.
Firstly, the proportion of the population which receives reimbursement gives a first indication on the presence and size of the affordability gap. If no coverage is present or only for a part of the population then an affordability gap is likely to exist in the market. Reimbursement remains the most stable and desirable access pathway as it is established in the healthcare system and supported by the authorities.
Additionally, the time until full/partial reimbursement is granted can lead to an interim affordability gap. Whilst a short delay to reimbursement (e.g. less than one year) is often normal, in cases of significant delays (such as more than 2 years) there is an interim gap in affordability which may be addressed by an affordability solution.
Finally, alongside reimbursement, alternative access routes might alleviate affordability gaps, or even address them depending on their reach. For example, patients can receive drugs via the judicial route in some markets, primarily in Latin America; whilst supporting access for select patients, pursuing the judicial route can be associated with a high administrative burden on patients, physicians, and affiliate teams (e.g., to submit the request and address the scrutiny from the court system), which makes it primarily suitable for rare diseases with high unmet need. Similarly, large-scale donation programs can eliminate the financial burden for the lowest-income groups, and thus reduce the need for affordability solutions.
Defining the solution
Once the presence of an interim or long-term affordability gap has been established, the next step is to match the solution to the local need. Various types of solutions exist which can broadly be divided into loyalty programs, brand solutions, differential pricing, and microfinancing.
Loyalty programs are commonly used and typically involve a discount scheme which supports access; the most common design is cost sharing, which can involve a simple discount (via a coupon) or a "Buy X Get Y Free" structure.
Brand solutions are strategies that tailor the brand to the market with affordability requirements in mind; this can involve a dual brand strategy (e.g. launching a cheaper brand in the OOP sector) or a non-premium brand (only launching one, discounted brand in the market).
Differential pricing involves the discounting of drugs in line with the individual’s financial situation, thus enabling tiered or varied discounts following a financial assessment (often conducted by a third party).
Microfinancing alleviates patients' financial pressure by enabling the payment of treatment costs in instalments.
Designing the solution
When designing a solution, first, any specific product characteristics need to be evaluated. Consequently, legal/regulatory constraints, external factors, and internal capabilities need to be assessed as these directly impact the viability of different solutions. Finally, the financial implications of the designed solution need to be evaluated.
Product characteristics: The specific features of the drug/treatment should guide solution design. For example, a solution for an acute treatment might benefit from microfinancing as it allows patients to pay in instalments rather than one large lump sum, whilst in a chronic drug with regular payments microfinancing could likely only be used to support patients with temporary dips in income due to unemployment, illness, etc. Alternatively, a solution for a drug primarily dispensed through hospitals will likely require close collaboration with hospital groups and prescribers, which will impact the structure of the program.
Legality: Laws relating to affordability solutions vary hugely between markets. For instance, some markets prohibit the direct promotion of pharmaceuticals to patients, making affordability solutions unsuitable. Other markets might have legal restrictions against one pharmaceutical company owning two brands for the same INN, ruling out a dual brand strategy.
External feasibility: The consideration of factors in the local environment should include precedence in the market, presence of a suitable third-party partner (e.g., retail pharmacies, 3rd party administrators, charities/NGOs) to implement the program, impact on the product in other markets through IRP, and cross-border sales (influencing the appropriate level of discounts).
Internal capabilities: Prior experience and resources of affiliates can impact which solutions are feasible. For example, does the company have the internal capacity and resources to manage programs, or market reputation to exit the strategy when appropriate.
Financial assessment: The impact of the chosen discount level on patient access and affordability but also financial viability for the company needs to be assessed. This should include an evaluation of the market size, resource requirements, and revenue potential.
Real-world example
An example of an implemented affordability solution is Takeda’s patient assistance program (PAP) for its I&I drug Entyvio, which has been offered in multiple countries, including Malaysia, Brazil, and the UAE, and reached hundreds of patients. As part of this scheme, the patient's financial situation is assessed to develop a suited payment plan, in a combination of cost sharing and differential pricing. This is done in partnership with a third-party organization (Axios International) which handles the day-to-day operations, financial assessment, promotion of the program, and delivery of free medicines. Patients without the ability to pay for included medicines can be supported through finding additional support from organisations such as charities or NGOs.
Windrose's take
Affordability solutions are becoming increasingly common as a tool for pharmaceutical companies to increase patient access and affordability, notably in emerging markets.
These solutions can indirectly maximize reimbursement potential, as access in the OOP sector can increase advocacy from patients and prescribers and enable evidence generation.
The programs are generally used to complement reimbursement and thus can be used in the short- or long-term depending on when/if reimbursement is granted, and what portion of the population is covered.
Companies need to consider the local environment namely legality, regulations, risk of cross-border sales, and feasibility, in conjunction with strategic considerations in terms of the financial and resource commitment required to support such a program.
Because of the immense importance of local dynamics, global teams will need to collaborate closely with local teams to ensure in-depth understanding and analysis of the market-specific situation in order to design truly market-relevant solutions.
Affordability solutions are not intended to be the sole tool enabling patient access, instead they form part of the ‘overall access puzzle’ alongside public/private reimbursement (which typically remains the preferred access route), judicial access (where appropriate), and donation programs.
Improving patient access to medicines - Affordability solutions as part of the puzzle
Article written by Kristina Funk (Left), Amy Morgan (Centre) and Mattia Belloni (Right), Windrose Consulting Group